
scroll down
Visceral leishmaniasis is particularly common in children, who responded very well to this new treatment. It also significantly lowered the risk of post-kala-azar dermal leishmaniasis (PKDL), a common complication of visceral leishmaniasis after treatment; PKDL affected 21% of patients following treatment with sodium stibogluconate but only 4% of patients after miltefosine and paromomycin. As PKDL patients are a source of infection, use of miltefosine and paromomycin could therefore also reduce transmission of Leishmania parasites.
These results are informing the activities of the follow-up EDCTP-funded LeishAccess project, which is facilitating the updating of visceral leishmaniasis treatment policy in countries in eastern Africa. Despite some progress, an estimated 50% of patients still do not have access to appropriate diagnosis and treatment. The LeishAccess consortium is sharing the new evidence with ministries of health in endemic countries and liaising with the WHO Guidelines Development Group, which is expected to produce updated treatment guidelines for visceral leishmaniasis towards the end of 2023.
Visceral leishmaniasis, due to infection with single-celled Leishmania parasites, is the second largest parasite infection after malaria. It is a particular challenge in countries in north and east Africa.
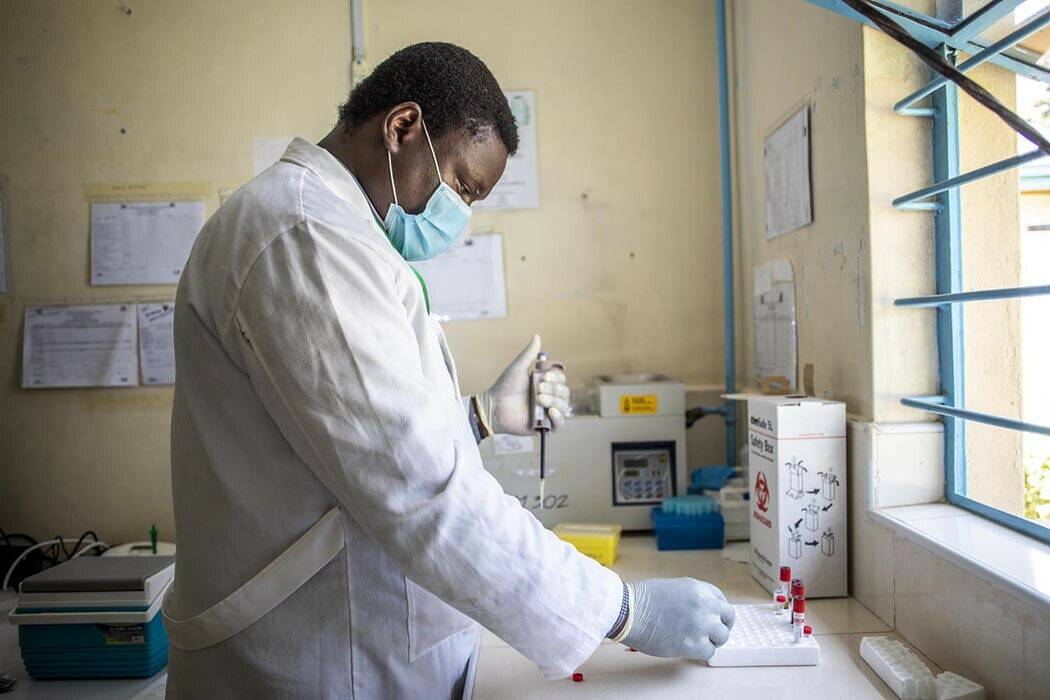
Standard treatment is with a combination of two drugs, sodium stibogluconate and paromomycin, given for 17 days. However, this involves painful daily injections and there is a risk of serious adverse reactions. In a trial spanning seven sites in four East African countries and with more than 400 participants, the AfriKADIA project compared this existing approach with a new treatment, a combination of two drugs, miltefosine and paromomycin, 32 given for 14 days. The new combination was 91% effective, at least as good as the current treatment, and reduced time in hospital by 18%.
The AfriKADIA project has shown that a novel therapy for visceral leishmaniasis is as effective as current treatments and much easier to administer.
A new treatment for visceral leishmaniasis
