One important analysis arose from an observation made in Rwanda, where the results from a widely used test, Xpert MTB/RIF, were frequently different when patients were tested more than once. A reanalysis of data revealed a high proportion of false positives – the test was incorrectly indicating the presence of drug-resistant bacteria. In a setting of low prevalence of drug resistance, almost half of cases detected (47%) were not in reality drug-resistant.
The most likely reason was low levels of bacteria in the samples used for diagnosis. The test interprets an absence of signal as evidence of resistance, whereas it may be due to limited quantities of pathogen TB for amplification.
These findings have important implications for how the Xpert test is used to inform clinical decision-making, as patients may be unnecessarily switched to a drug regime for multidrug-resistant TB. The results were communicated to WHO and informed the development of guidelines on TB diagnosis.
The findings highlight the importance of studying innovative new technologies within the health systems of countries, to ensure that evidence is of direct relevance to country decision-makers.

scroll down
It is important that TB patients with drug-resistant infections are identified as rapidly as possible, so that they can be placed on the appropriate treatment. Standard culture methods to detect resistant infections are very slow, so there is increasing use of molecular diagnostics that can rapidly detect resistance mutations, particularly those conferring resistance to rifampicin. However, how best to use these tools in routine care has yet to be established.
Working within the health systems of nine African countries, the DIAMA project is exploring how a range of tools for detecting multidrug-resistant TB could be implemented, either at the local level or within central facilities. The Deeplex® Myc-TB test, based on targeted next generation sequencing, was implemented in reference labs in Rwanda and Benin, and the data generated contributed to endorsement of the test by WHO.
The DIAMA project has generated important data on the detection of drug-resistant TB, informing WHO recommendations on TB diagnosis.
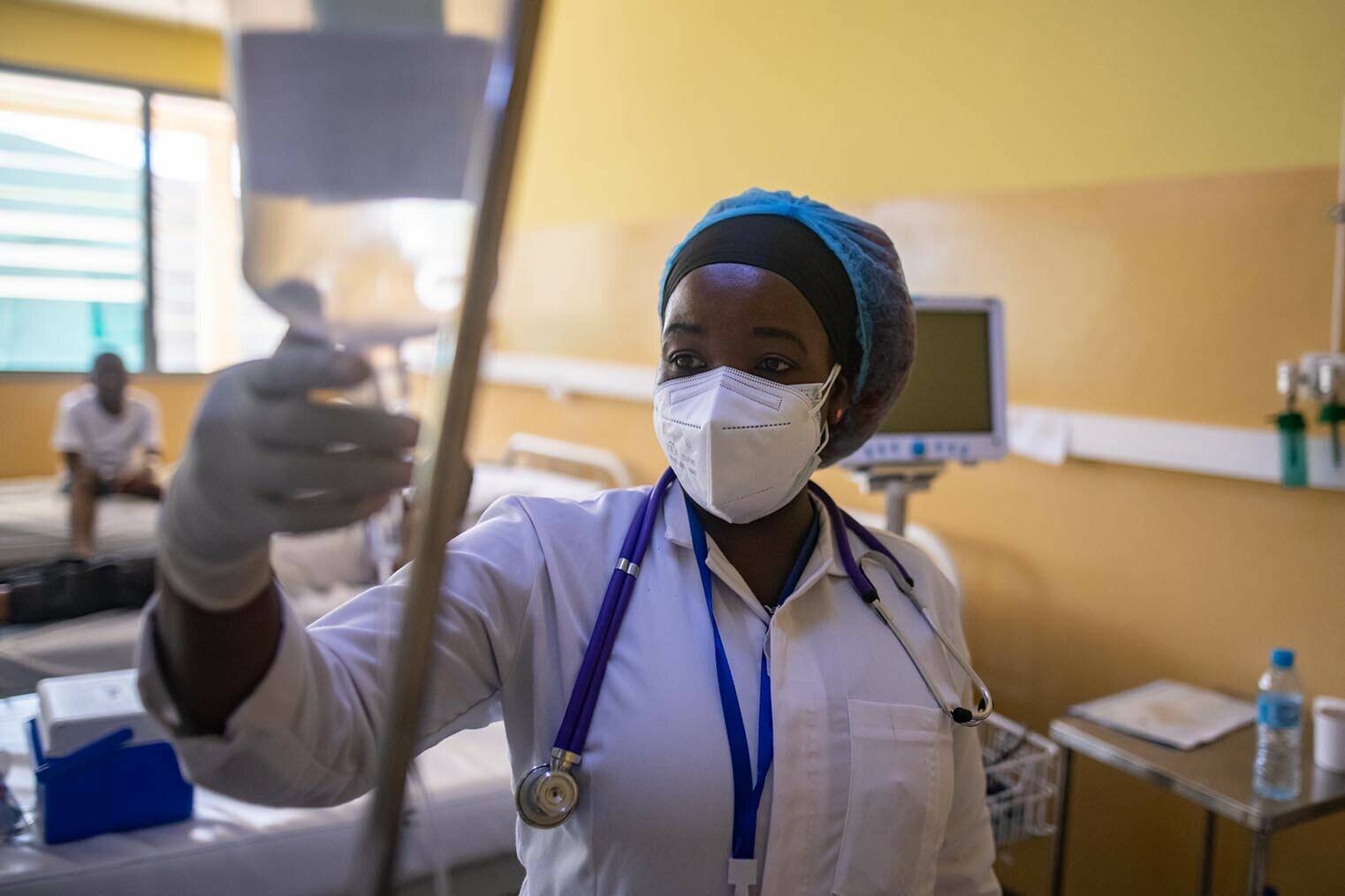
Detecting drug-resistant TB